When Amelie Darblade relocated from France to Vancouver seven years ago, she fell ill and went to see an English-speaking physician. The experience was a stark reminder of the communication challenges faced by people whose first language isn’t English.
“I understood most of the session, but could not understand a word related to my condition,” said Amelie. “The physician wrote the name of the condition on a piece of paper for me. I went home and Googled it – the results were a little dramatic.”
 “Medical terms and stress will challenge patients’ English proficiency in a health-care environment,” adds Amelie, who is now a virtual health leader at the Office of Virtual Health, working on the Virtual Interpreting strategy to support patients that don't have English as a primary language.
“Medical terms and stress will challenge patients’ English proficiency in a health-care environment,” adds Amelie, who is now a virtual health leader at the Office of Virtual Health, working on the Virtual Interpreting strategy to support patients that don't have English as a primary language.
Language barriers can cause a number of challenges during a medical appointment. People who are Deaf, Deaf-Blind, Hard of Hearing or have a Language Other Than English (LOTE) can misunderstand key medical information, which can lead to frustration for patients, as well as confusion with care plans. Many patients bring family members or friends to act as an interpreter, yet they may not be able to interpret the medical terminology, and it doesn’t provide patients with the medical autonomy they’re entitled to.
A pilot project of a virtual interpreting tool at Vancouver Coastal Health in 2020 showed that the length of stay in clinics for people who have LOTE is, on average, longer than English speaking patients. Improving access to interpreters using virtual tools reduced LEP patients’ length of stay.
“Using a tool that bridges the communication between patient and provider has a reciprocal benefit because it means a provider gets accurate health information from the patient and the patient gets accurate care information from the provider. It also supports a Deaf or Hard of Hearing patient’s right to have an American Sign Language interpreter present in a medical appointment,” said Kiran Malli, director of Provincial Language Service.
- Video Remote Interpreting (VRI): Provides on-demand access to 240 languages, including American Sign Language 24/7, when a patient and health-care provider meet in person.
- Interpreting services during virtual health visits: A provider can submit a request to Provincial Language Service to have an interpreter that connects to their one-to-one or group virtual health visit.
- Closed captioning during Zoom for Healthcare virtual health visits: Option for automatic live transcription, or professional captioners/transcribers are available.
Learn more about the above virtual communication tools in this infographic, and learn how to book these services for patients on the Provincial Language Service page.
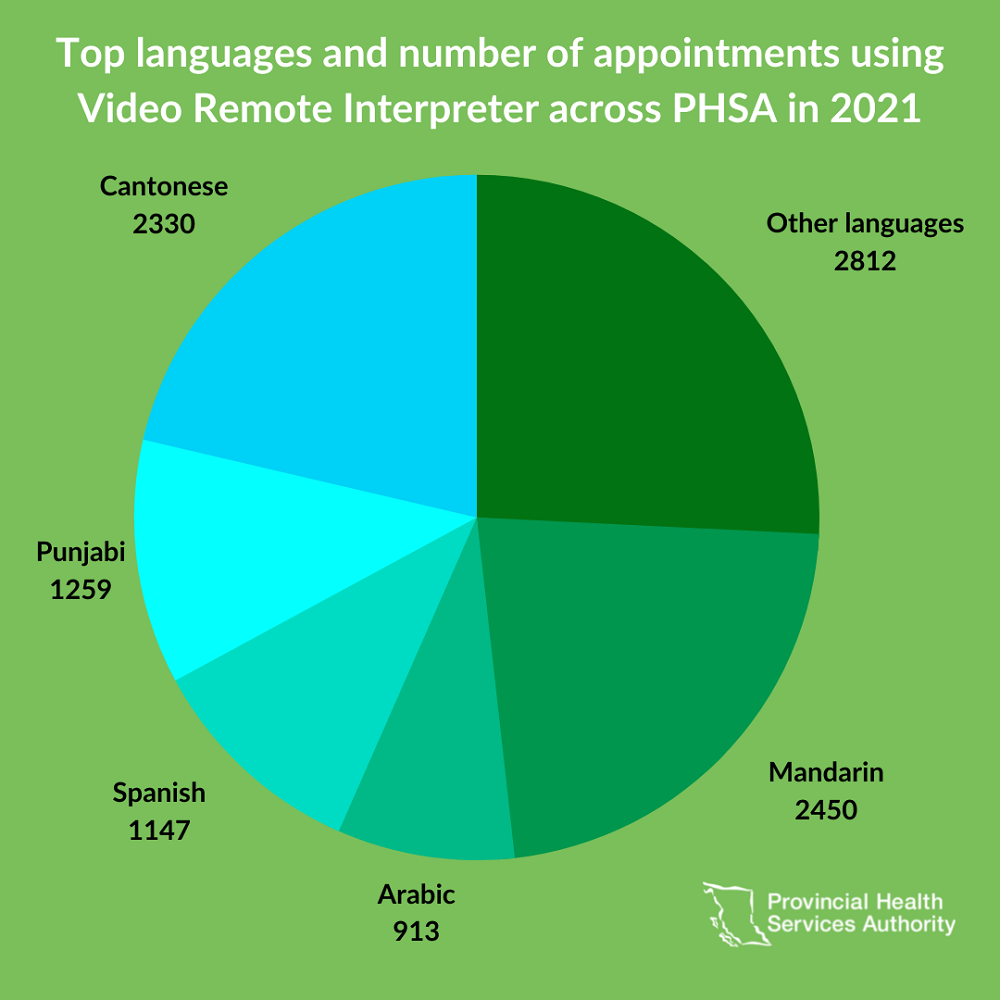
In 2019, VRI was successfully introduced at a BC Cancer ambulatory clinic. Use expanded to additional clinics at PHSA, Fraser Health and Vancouver Coastal Health.
In 2020, a VRI app was installed on iPhones in BCEHS ambulances enabling paramedics to access ASL interpreters so they can communicate in real time with patients.
In January 2022, Interior Health implemented their first VRI device at Penticton Regional Hospital. In early April, VRI was rolled out at the Royal Inland Hospital in Kamloops.
If a health-care provider is aware of a language or communication barrier with a patient, it is the provider’s responsibility to ensure the appropriate communication tools are available for the appointment. This will help the provider communicate with the patient directly without depending on the patient’s family/friends or volunteers to act as interpreters.
Amelie’s experience happened before VRI was introduced to clinics in the Lower Mainland. Her subsequent appointment was attended by an interpreter. “The session included an examination and it was awkward with the interpreter in the room. It would have been more comfortable having a remote Interpreter through VRI – and the ability to use it in privacy mode.”
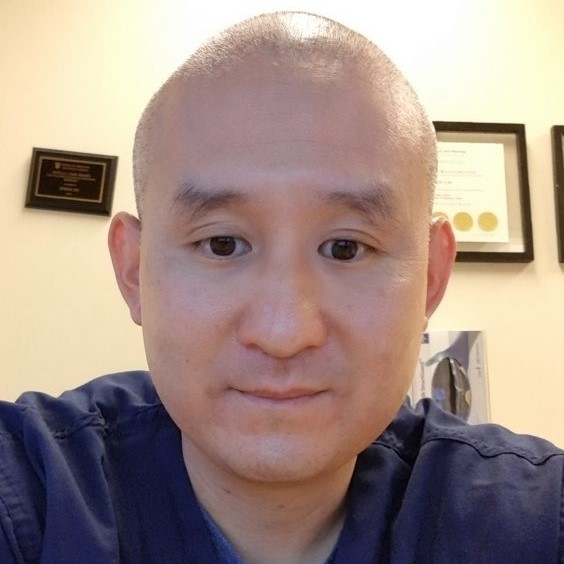 Before closed captioning was enabled for Zoom for Healthcare users in December 2021, Jowan Lee, professional practice lead at St Paul’s Hospital, and his colleagues communicated with patients by typing in the chat area of Zoom, which was prone to errors and inefficient.
Before closed captioning was enabled for Zoom for Healthcare users in December 2021, Jowan Lee, professional practice lead at St Paul’s Hospital, and his colleagues communicated with patients by typing in the chat area of Zoom, which was prone to errors and inefficient.
For in-person visits in the clinic, they used speech-to-text apps on their iPhones and tablets, and held them up for the patients to read. “Closed captioning on Zoom makes communication so much easier because it’s hands free, it’s smooth and it’s reasonably accurate,” said Jowan.
“Clinicians report having higher patient engagement when they use communication tools that bridge the language gap,” adds Kiran. “Patient satisfaction and health outcomes increase because they have the accurate information they need and feel empowered.”
PHSA’s Office of Virtual Health and Provincial Language Service are working on a Virtual Interpreting Provincial Expansion project, which promotes the adoption of virtual health tools that improve patient access to care, particularly for patients who have a LOTE or are Deaf, Deaf-Blind, or Hard of Hearing.
On April 20 and 23, Provincial Language Service will host focus groups for Deaf, Deaf-Blind and Hard of Hearing patients to provide feedback on how VRI impacted their health-care experience. Learn more about the focus group.
- The need for an interpreter and the language required to communicate with the patient must be noted in the patient record. Refusal of a Qualified Interpreter by a patient must also be noted in the patient record in addition to what type of language resource was used (e.g. family), as outlined in the PHSA Language Access Policy.
- Access interpreting services and integrate accessibility tools into your services at the Provincial Language Service webpage. Accessibility tools augment Provincial Language Service’s other interpreter offerings, which include in-person and over-the-phone interpreting.
- Access automatic and live captioning for virtual health visits at the Zoom for Healthcare webpage.
- The Provincial Virtual Health leads and provides strategic direction for the virtual health initiative at PHSA.