At the heart of stroke care is the individual—a person navigating prevention, acute treatment, and recovery. Empowering individuals with knowledge about stroke risk factors, symptoms and the importance of timely FAST (Face, Arms, Speech, Time) sign recognition and treatment can save lives.
Likewise, health care providers who are informed on best practices and collaborate effectively across disciplines contribute to seamless, patient-centered care.
The stroke care continuum is frequently described in a way that depicts the onset or first signs of a stroke as the "start," however, with 80% of strokes being preventable, it's important for us to recognize prevention as the true start of the stroke care continuum.
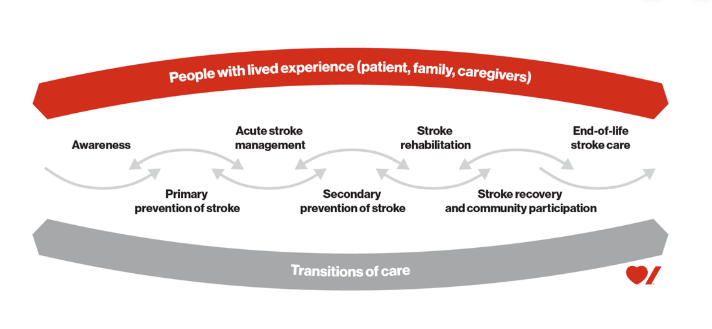 The stroke care continuum
The stroke care continuum
The primary and secondary prevention methods are much like many of us have heard before: knowing your risk and leading a healthy, balanced lifestyle through healthy eating, being active and living smoke free. Health care providers, health authorities and health organizations alike sound like a broken record when stating the importance of these prevention methods, but their impacts in preventing stroke are too tangible to avoid repeating. Nine in 10 Canadians have at least one risk factor for stroke, some modifiable, some out of our control. Taking charge of your modifiable risk factors is empowering, and can relieve yourself, your family and your community of the deeply felt effects of a stroke.

“The Heart and Stroke Foundation of Canada’s 2019 Report on Heart, Stroke and Vascular Cognitive Impairment illustrated that strokes cost the Canadian economy $3.6 billion a year in physician services, hospital costs, lost wages and decreased productivity. In a time where our country is trying to identify cost-saving and GDP-bolstering opportunities, stroke prevention can play a great role,” shares Sacha Arsenault, provincial director, Stroke Services BC.
 Stroke affects not just the brain, but the whole person, as it often comes with several, short- to long-term physical, cognitive and emotional side effects of varying severity. New research is even pointing to the connection between stroke and dementia. The treatment and rehabilitation stages clearly demonstrate the breadth of a stroke’s impacts. A gold-standard stroke unit care team, as laid out in BC’s Stroke Quality Standard, consists of physicians, nurses, occupational therapists, physiotherapists, speech-language pathologists, pharmacists, social workers, and dietitians. The coordinated efforts of these professionals maximize recovery potential and reduce the likelihood of death and disability by as much as 30 per cent.
Stroke affects not just the brain, but the whole person, as it often comes with several, short- to long-term physical, cognitive and emotional side effects of varying severity. New research is even pointing to the connection between stroke and dementia. The treatment and rehabilitation stages clearly demonstrate the breadth of a stroke’s impacts. A gold-standard stroke unit care team, as laid out in BC’s Stroke Quality Standard, consists of physicians, nurses, occupational therapists, physiotherapists, speech-language pathologists, pharmacists, social workers, and dietitians. The coordinated efforts of these professionals maximize recovery potential and reduce the likelihood of death and disability by as much as 30 per cent.
This breadth of care also highlights why ongoing education and collaboration among health care providers are critical. Recognizing the uniquely large number of providers involved in stroke care, Stroke Services BC is committed to keeping the BC health care community up to date by sharing best practices and the latest evidence, offering providers monthly education opportunities and fostering collaboration among key partner organizations.
 "Ongoing education is vital for stroke care, where practices are continually evolving and collaboration is key. Our monthly education sessions cover topics across the stroke continuum and feature expert speakers from across the province, ensuring providers stay informed and connected to best practices,” says Alison DeWit, clinical nurse specialist, Stroke Services BC.
"Ongoing education is vital for stroke care, where practices are continually evolving and collaboration is key. Our monthly education sessions cover topics across the stroke continuum and feature expert speakers from across the province, ensuring providers stay informed and connected to best practices,” says Alison DeWit, clinical nurse specialist, Stroke Services BC.
This work can enhance the patient experience and improve outcomes.
Together, individuals, families, and the diverse stroke care team create a robust support system throughout the stroke care continuum, starting with prevention and extending through acute care to rehabilitation. By working together and empowering individuals, we can reduce stroke risk, improve outcomes, and enhance quality of life for those affected by stroke. Everyone—patients, families, healthcare providers—plays a significant role along this journey.
